Trends in Intensive Care Admissions and Outcomes of Stroke Patients Over 10 Years in Brazil: Impact of the COVID-19 Pandemic
Pedro Kurtz 1, Leonardo S L Bastos 2, Fernando G Zampieri 3, Gabriel R de Freitas 4, Fernando A Bozza 5, Marcio Soares 6, Jorge I F Salluh 7
Chest. 2023 Mar;163(3):543-553. doi: 10.1016/j.chest.2022.10.033. Epub 2022 Nov 5.PMID: 36347322 Free PMC article.
Abstract
Background: The coronavirus 2019 (COVID-19) pandemic affected stroke care worldwide. Data from low- and middle-income countries are limited.
Research question: What was the impact of the pandemic in ICU admissions and outcomes of patients with stroke, in comparison with trends over the last 10 years?
Study design and methods: Retrospective cohort study including prospectively collected data from 165 ICUs in Brazil between 2011 and 2020. We analyzed clinical characteristics and mortality over a period of 10 years and evaluated the impact of the pandemic on stroke outcomes, using the following approach: analyses of admissions for ischemic and hemorrhagic strokes and trends in in-hospital mortality over 10 years; analysis of variable life-adjusted display (VLAD) during 2020; and a mixed-effects multivariable logistic regression model.
Results: A total of 17,115 stroke admissions were analyzed, from which 13,634 were ischemic and 3,481 were hemorrhagic. In-hospital mortality was lower after ischemic stroke as compared with hemorrhagic (9% vs 24%, respectively). Changes in VLAD across epidemiological weeks of 2020 showed that the rise in COVID-19 cases was accompanied by increased mortality, mainly after ischemic stroke. In logistic regression mixed models, mortality was higher in 2020 compared with 2019, 2018, and 2017 in patients with ischemic stroke, namely, in those without altered mental status. In hemorrhagic stroke, the increased mortality in 2020 was observed in patients 50 years of age or younger, as compared with 2019.
Interpretation: Hospital outcomes of stroke admissions worsened during the COVID-19 pandemic, interrupting a trend of improvements in survival rates over 10 years. This effect was more pronounced during the surge of COVID-19 ICU admissions affecting predominantly patients with ischemic stroke without coma, and young patients with hemorrhagic stroke.
Keywords: COVID-19 pandemic; coronavirus 2019; hemorrhagic; ischemic; outcomes; stroke.
Copyright © 2022 American College of Chest Physicians. Published by Elsevier Inc. All rights reserved.
Non-COVID-19 intensive care admissions during the pandemic: a multinational registry-based study
Joshua McLarty 1 2, Edward Litton 3 4, Abigail Beane 5 6, Diptesh Aryal 7, Michael Bailey 2, Stepani Bendel 8 9, Gaston Burghi 10, Steffen Christensen 11, Christian Fynbo Christiansen 12, Dave A Dongelmans 13 14, Ariel L Fernandez 15, Aniruddha Ghose 16, Ros Hall 17, Rashan Haniffa 5 6, Madiha Hashmi 18, Satoru Hashimoto 19 20, Nao Ichihara 21, Bharath Kumar Tirupakuzhi Vijayaraghavan 22 23, Nazir I Lone 24, Maria Del Pilar Arias López 25 26, Mohamed Basri Mat Nor 27, Hiroshi Okamoto 28, Dilanthi Priyadarshani 29, Matti Reinikainen 8 9, Marcio Soares 30, David Pilcher 31 2, Jorge Salluh 30 32; Linking of Global Intensive Care (LOGIC) Collaboration
Abstract
Background: The COVID-19 pandemic resulted in a large number of critical care admissions. While national reports have described the outcomes of patients with COVID-19, there is limited international data of the pandemic impact on non-COVID-19 patients requiring intensive care treatment.
Methods: We conducted an international, retrospective cohort study using 2019 and 2020 data from 11 national clinical quality registries covering 15 countries. Non-COVID-19 admissions in 2020 were compared with all admissions in 2019, prepandemic. The primary outcome was intensive care unit (ICU) mortality. Secondary outcomes included in-hospital mortality and standardised mortality ratio (SMR). Analyses were stratified by the country income level(s) of each registry.
Findings: Among 1 642 632 non-COVID-19 admissions, there was an increase in ICU mortality between 2019 (9.3%) and 2020 (10.4%), OR=1.15 (95% CI 1.14 to 1.17, p<0.001). Increased mortality was observed in middle-income countries (OR 1.25 95% CI 1.23 to 1.26), while mortality decreased in high-income countries (OR=0.96 95% CI 0.94 to 0.98). Hospital mortality and SMR trends for each registry were consistent with the observed ICU mortality findings. The burden of COVID-19 was highly variable, with COVID-19 ICU patient-days per bed ranging from 0.4 to 81.6 between registries. This alone did not explain the observed non-COVID-19 mortality changes.
Interpretation: Increased ICU mortality occurred among non-COVID-19 patients during the pandemic, driven by increased mortality in middle-income countries, while mortality decreased in high-income countries. The causes for this inequity are likely multi-factorial, but healthcare spending, policy pandemic responses, and ICU strain may play significant roles.
Keywords: COVID-19; Clinical Epidemiology; Critical Care.
© Author(s) (or their employer(s)) 2023. No commercial re-use. See rights and permissions. Published by BMJ.
Conflict Of Interest Statement
Competing interests: DP and Dr EL are members of the Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcome and Resources Evaluation management committee. AB is funded by Wellcome. JS and MS are cofounders and shareholders of Epimed Solutions, a healthcare cloud-based analytics company. They are also supported in part by individual research grants from CNPq and FAPERJ. SB is the current chair, and MR is the past chair of the Finnish Intensive Care Consortium (both unpaid). DAD is unpaid chair of NICE foundation. NI’s primary affiliation is the Department of Healthcare Quality Assessment, which is a social collaboration department at the University of Tokyo supported by National Clinical Database, Johnson & Johnson K.K., and Nipro corporation. BKTV is the National Coordinator for the Indian Registry of IntenSive care (IRIS) and is supported for 0.5 FTE by funding from the Wellcome Trust, UK. The remaining authors have no conflicts of interest to declare.
Worldwide Clinical Intensive Care Registries Response To The Pandemic: An International Survey
Dave A Dongelmans 1, Amanda Quintairos 2, Eirik Alnes Buanes 3, Diptesh Aryal 4, Sean Bagshaw 5, Stepani Bendel 6, Joe Bonney 7, Gaston Burghi 8, Eddy Fan 9, Bertrand Guidet 10, Rashan Haniffa 11, Madiha Hashimi 12, Satoru Hashimoto 13, Nao Ichihara 14, Bharath Kumar Tirupakuzhi Vijayaraghavan 15, Nazir Lone 16, Maria Del Pilar Arias Lopez 17, Mohd Zulfakar Mazlam 18, Hiroshi Okamoto 19, Andreas Perren 20, Kathy Rowan 21, Martin Sigurdsson 22, Wangari Silka 23, Marcio Soares 24, Grazielle Viana 25, David Pilcher 26, Abigail Beane 27, Jorge I F Salluh 24
No abstract available
Conflict Of Interest Statement
Declaration of Competing Interest Drs Salluh and Soares are co-founders and shareholders of Epimed Solutions, a cloud-based analytics company. Dr. D.A. Dongelmans is unpaid chair of NICE foundation. The other authors declare that they have no conflicts of interest.
- Brazilian ICUs project http://www.utisbrasileiras.com.br/uti-adulto/caracteristicas-das-utis-pa… Available from. (accessed on March 20th, 2022)
- Estenssoro E., Loudet C.I., Ríos F.G., Kanoore Edul V.S., Plotnikow G., Andrian M., et al. Dubin a; SATI-COVID-19 study group. Clinical characteristics and outcomes of invasively ventilated patients with COVID-19 in Argentina (SATICOVID): a prospective, multicentre cohort study. Lancet Respir Med. 2021 Sep;9(9):989–998. – PMC – PubMed
- CRIT Care Asia, Hashmi M., Beane A., Murthy S., Dondorp A.M., Haniffa R. Leveraging a cloud-based critical care registry for COVID-19 pandemic surveillance and research in low- and middle-income countries. JMIR Public Health Surveill. 2020 Nov 23;6(4) e21939. – PMC – PubMed
- https://www.icubenchmarking.com/#wowheare (accessed on March 20th, 2022)
- Aryal D., Beane A., Dondorp A.M., Green C., Haniffa R., Hashmi M., et al. Operationalisation of the Randomized Embedded Multifactorial Adaptive Platform for COVID-19 trials in a low and lower-middle income critical care learning health system. Wellcome Open Res. 2021 Jan 28;6:14. – PMC – PubMed
Learning Systems As A Path To Improve ICU Staff Wellbeing
References
- Endacott R., Pearce S., Rae P., et al. How COVID-19 has affected staffing models in intensive care: a qualitative study examining alternative staffing models (SEISMIC) J Adv Nurs. 2022;78(4):1075–1088. – PubMed
- Azoulay E., Pochard F., Reignier J., et al. Symptoms of mental health disorders in critical care physicians facing the second COVID-19 wave: a cross sectional study. Chest. 2021;160(3):944–955. – PMC – PubMed
- Lone N., McPeake J., Stewart N.I., et al. Influences of socioeconomic deprivation on interventions and outcomes for patients admitted with COVID-19 to critical care unit in Scotland: a national cohort study. Lancet Reg Health Eur. 2021;1:100005. – PMC – PubMed
- Lobo S.M., Creutzfeldt C.J., Maia I.S., et al. Perceptions of critical care shortages, resource use and provider well-being during the COVID-19 pandemic: a survey of 1,985 health care providers in Brazil. Chest. 2022;161(6):1526–1542. – PMC – PubMed
- Kerlin M.P., McPeake J., Mikkelsen M.E. Burnout and joy in the profession of critical care medicine. Crit Care. 2020;24:98. – PMC – PubMed
Get To Know LOGIC: The World’s Largest Intensive Care Benchmarking Platform
LOGIC (Linking of Global Intensive Care) is an independent consortium of databases of large ICU networks and national records of quality in intensive care medicine. LOGIC aims to connect ICUs to promote quality improvement through international benchmarking and collaborative research, assisting in data-driven decision-making.
The project brings together some of the largest national records databases in the world. Through a shared online platform, researchers and ICU networks have easy access to aggregated data on ICU admissions worldwide, and to information updated annually.
LOGIC’s international benchmarking is a powerful assessment tool in intensive care and quality improvement, where all users of participating networks can compare the performance of ICUs and thus, increase epidemiology and outcome knowledge.
Logic is currently present in more than 13 countries, such as Brazil, Uruguay, The Netherlands, India, Australia, France, among others, with more than 2,000 ICUs monitored, adding more than 7 million admissions to these units since the beginning of the project, which offers an international approach to ICU benchmarking in a pragmatic and valuable way for physicians and researchers.
A Pooled Analysis Of Four Observational Studies
Geoeconomic variations in epidemiology, ventilation management, and outcomes in invasively ventilated intensive care unit patients without acute respiratory distress syndrome: a pooled analysis of four observational studies.
Pisani L, Algera AG, Neto AS, Azevedo L, Pham T, Paulus F, de Abreu MG, Pelosi P, Dondorp AM, Bellani G, Laffey JG, Schultz MJ; ERICC study investigators; LUNG SAFE study investigators; PRoVENT study investigators; PRoVENT-iMiC study investigators.
Abstract
Background: Geoeconomic variations in epidemiology, the practice of ventilation, and outcome in invasively ventilated intensive care unit (ICU) patients without acute respiratory distress syndrome (ARDS) remain unexplored. In this analysis we aim to address these gaps using individual patient data of four large observational studies.
Methods: In this pooled analysis we harmonised individual patient data from the ERICC, LUNG SAFE, PRoVENT, and PRoVENT-iMiC prospective observational studies, which were conducted from June, 2011, to December, 2018, in 534 ICUs in 54 countries. We used the 2016 World Bank classification to define two geoeconomic regions: middle-income countries (MICs) and high-income countries (HICs). ARDS was defined according to the Berlin criteria. Descriptive statistics were used to compare patients in MICs versus HICs. The primary outcome was the use of low tidal volume ventilation (LTVV) for the first 3 days of mechanical ventilation. Secondary outcomes were key ventilation parameters (tidal volume size, positive end-expiratory pressure, fraction of inspired oxygen, peak pressure, plateau pressure, driving pressure, and respiratory rate), patient characteristics, the risk for and actual development of acute respiratory distress syndrome after the first day of ventilation, duration of ventilation, ICU length of stay, and ICU mortality.
Findings: Of the 7608 patients included in the original studies, this analysis included 3852 patients without ARDS, of whom 2345 were from MICs and 1507 were from HICs. Patients in MICs were younger, shorter and with a slightly lower body-mass index, more often had diabetes and active cancer, but less often chronic obstructive pulmonary disease and heart failure than patients from HICs. Sequential organ failure assessment scores were similar in MICs and HICs. Use of LTVV in MICs and HICs was comparable (42·4% vs 44·2%; absolute difference -1·69 [-9·58 to 6·11] p=0·67; data available in 3174 [82%] of 3852 patients). The median applied positive end expiratory pressure was lower in MICs than in HICs (5 [IQR 5-8] vs 6 [5-8] cm H2O; p=0·0011). ICU mortality was higher in MICs than in HICs (30·5% vs 19·9%; p=0·0004; adjusted effect 16·41% [95% CI 9·52-23·52]; p<0·0001) and was inversely associated with gross domestic product (adjusted odds ratio for a US$10 000 increase per capita 0·80 [95% CI 0·75-0·86]; p<0·0001).
Interpretation: Despite similar disease severity and ventilation management, ICU mortality in patients without ARDS is higher in MICs than in HICs, with a strong association with country-level economic status.
Funding: No funding.
Copyright © 2022 The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY 4.0 license. Published by Elsevier Ltd.. All rights reserved.
Conflict Of Interest Statement
Declaration of interests We declare no competing interests.
Development Of A Core Outcome Set For General Intensive Care Unit Patients – Need For A Broader Context?
Development of a core outcome set for general intensive care unit patients – need for a broader context?
Pari V, Beane A, Salluh JI, Donglemans DA.Acta Anaesthesiol Scand. 2022 Jan 28. doi: 10.1111/aas.14031. Online ahead of print.
by: The LOGIC Team
New International Benchmarking
The International Benchmarking Has Been Updated.
Check the news below:
New interface
The new layout brings forward a more practical navigation flux and allows for a more objective analysis of registrations from each country.
New Reports
The data can be visualized through more evolutionary and consolidated reports, thus, facilitating the analyses if indicators between registrations and years.
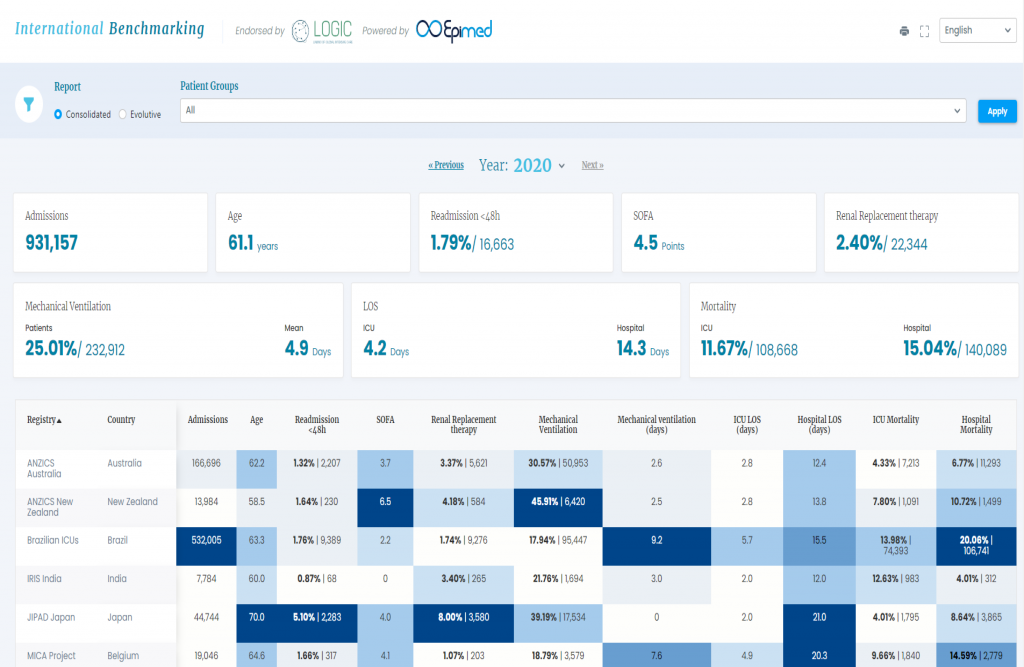
Consolidated Reports
- All present indicators will have a unique interface, allowing for better analyses and comparisons between registrations.
- Information about each participating registration with an access link to institutional sites.
- Navigation fields based on patient groups and years.
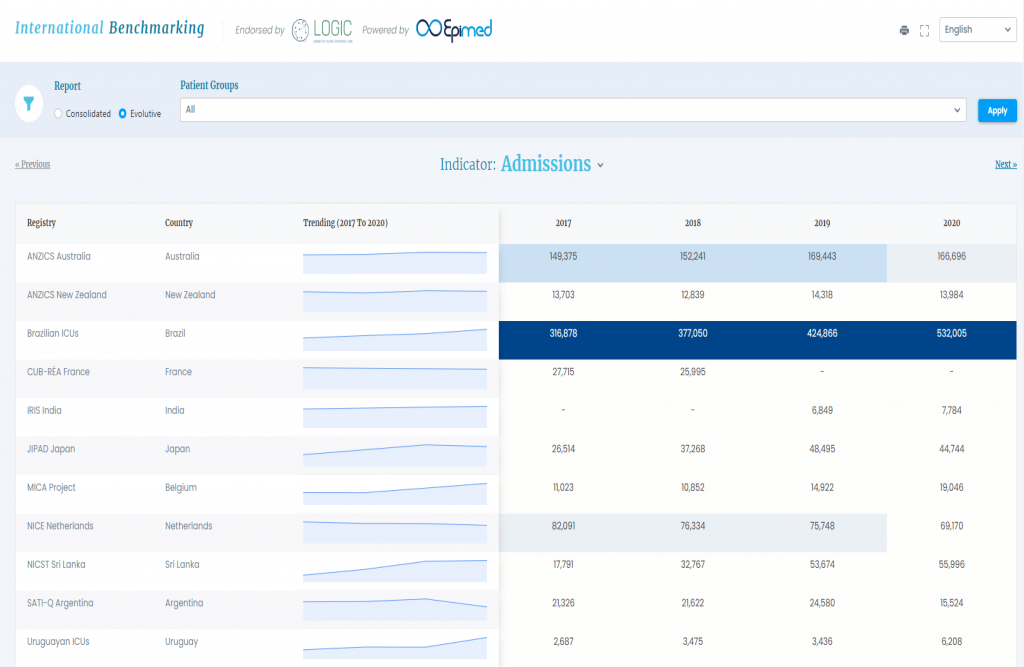
Evolutionary Reports
- Visualization of indicators with graphs and evolutionary tendency throughout the years.
- Navigation fields based on groups and patient indicators.
LOGIC – Linking Of Global Intensive Care
Our group is growing! We now represent 18 registries in 15 countries in Europe, The Americas, Oceania and Asia.
More than 6 Million ICU admissions in our benchmarking platform help you understand the results of your ICU, region of the world and your national registry.
New members from Europe and Asia will join us in the 2nd semester of 2021 and we are aiming to reach 20 countries!
The LOGIC benchmarking platform was just updated! All data from 2020 including COVID-19 patients is available and can be used by all registries. Thanks for the collaboration and trust in this project.
Check out the recent publications from LOGIC and from individual LOGIC members!
Time to Revisit Treatment Limitations in Critical Care Benchmarking.
Beane A, Dongelmans DA, Fernandez AL, Guidet B, Haniffa R, Arias Lopez MP, Pilcher D, Salluh J, Vijayaraghavan BKT; Linking of Global Intensive Care Collaboration (LOGIC).
Crit Care Med. 2021 Apr 1;49(4):e472-e473
A discussion on the implications of care limitations in outcomes of ICU patients and its interpretation for ICU performance evaluation.
A scoping review of registry captured indicators for evaluating quality of critical care in ICU.
Intensive care for COVID-19 in low- and middle-income countries: research opportunities and challenges.
Ongoing Research
We have finished a survey on how registries responded to the challenges of COVID-19. We were thrilled by the massive participation of current LOGIC members and other non-member registries! Results are being analyzed and will be published soon.
We are currently enrolling registries to a study on the impact of the pandemic on the case-mix and ICU performance as captured by national registries and large databases. Join us!
Join LOGIC and be a part of the only international and independent consortium for ICU benchmarking and quality improvement.
How To Evaluate Intensive Care Unit Performance During The COVID-19 Pandemic
Zampieri FG, Soares M, Salluh JIF.
Rev Bras Ter Intensiva. 2020 Jun;32(2):203-206. doi: 10.5935/0103-507x.20200040. Epub 2020 Jul 13.
by: The LOGIC Team
